Vertical and horizontal guided bone regeneration
in atrophic posterior mandible using a non-absorbable PTFE membrane with titanium reinforcement.
Dr. Javier Mayor Arenal
Specialist in oral surgery, implantology and periodontics
Madrid, Spain
Facts
Patient:
A 55-year-old woman with no relevant medical history.
Clinical problem:
The patient had peri-implantitis in implant 36, with symptoms of pain and suppuration in the area. She wanted a definitive solution, and was prescribed implant explantation treatment, and then regeneration of the resulting defect, so that a new implant could be placed and surrounded by bone.
Clinical solution:
We performed vertical and horizontal guided bone regeneration in the defect area using a titanium-reinforced PTFE membrane, adding approximately 90% autogenous bone with 10 to 15% xenograft of porcine hydroxyapatite. After maturation of the bone graft, we placed the implant 36 again, surrounded by bone.
Treatment plan:
- Perform vertical and horizontal guided bone regeneration.
- Use a NeoGen PTFE Non-absorbable membrane with titanium reinforcement for bone augmentation.
- Wait for new bone formation over a period of 9 to 12 months.
- Perform reentry into bone regeneration, removing the membrane, taking a bone cylinder (biopsy) to perform a histomorphometric analysis of the regenerated bone tissue, and place an implant in position 36 (the patient did not want to place implant 37).
- After 3 months, we performed soft tissue surgery to gain keratinized mucosa inserted into the implant area 36.
- After 3 months, we connected a healing device to implant 36.
- Subsequently, we placed the final rehabilitation on implant 36.
Products:
1 NeoGen Ti-Reinforced PTFE Membrane.
Conclusion:
Guided vertical and horizontal bone regeneration is a predictable and effective technique, provided that an appropriate work protocol is applied and quality biomaterials are used, which provide us with adequate maintenance of the space for a sufficient period of time, so that it is occupied by the newly formed bone, achieving regeneration of the defect, and obtaining vascularized and compact bone regeneration, which allows us to place the implants and their prosthetic rehabilitation.
step by step
step by step
-
Figure 1.
Panoramic X-ray showing peri-implantitis in the lower implants. Below on the left we see in more detail the bone loss in implant 36 due to peri-implantitis and on the right we see the bone defect resulting from its explantation.
-
Figure 2.
Clinical situation of healed hard and soft tissues after implant explantation 36
-
Figure 3.
Bone defect after elevating the mucoperiosteal flap. We made an incision in the center of the crest and scalloped intrasulcularly 3 teeth beyond the defect (avoiding making discharges where there were crowns), finally we made a vertical discharge incision at the anterior limit of the flap.
-
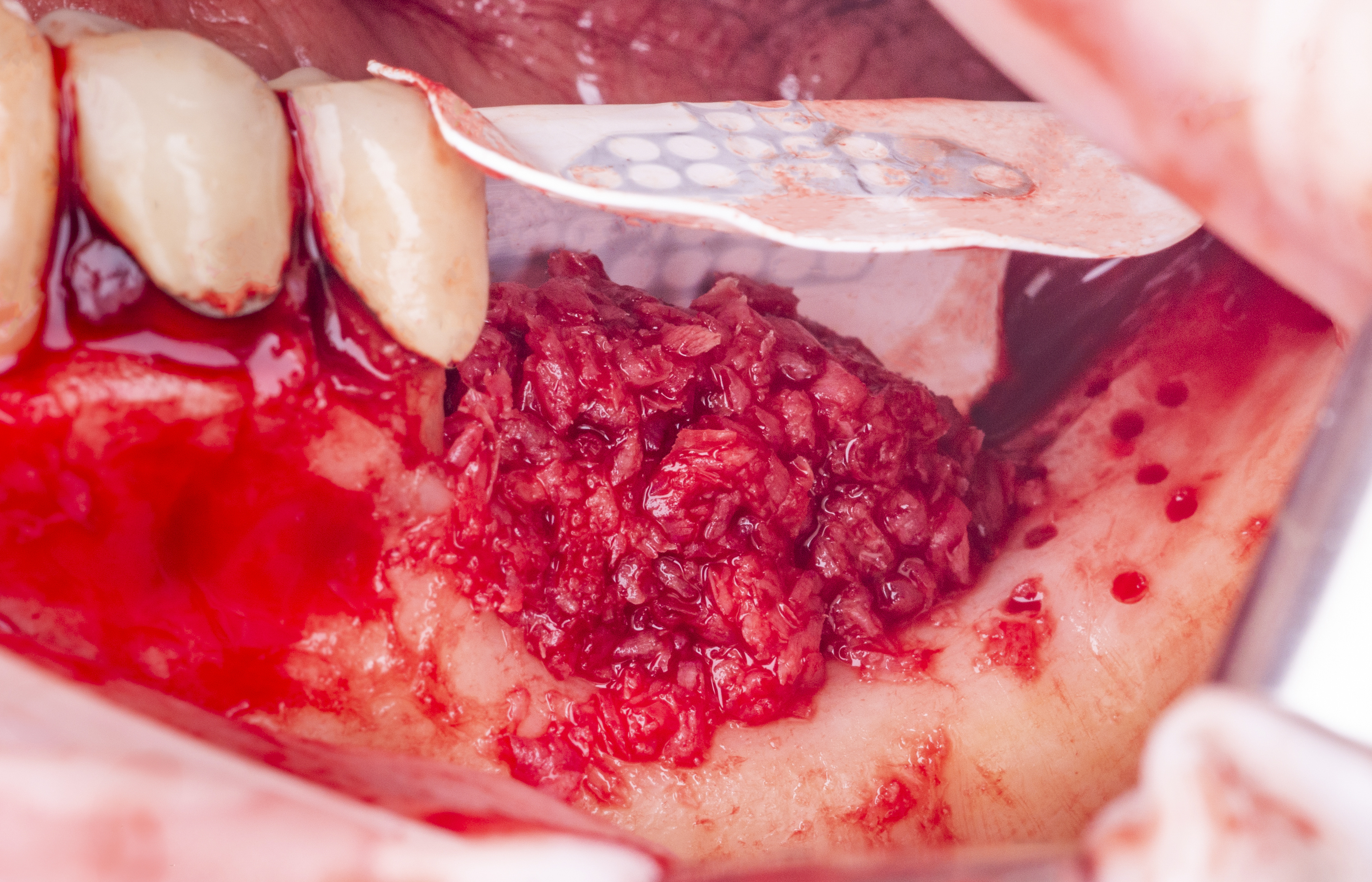
Figure 4.
We perform cortical perforations to promote vascularization and osteogenesis in the bone graft.
-
Figure 5.
We stabilize the NeoGen Ti-Reinforced PTFE Membrane, starting to fix it from the lingual and incorporating an autogenous graft into the defect in approximately 90% proportion, so that together with the extraordinary maintenance of space provided by this membrane, we achieve adequate new bone formation.
-
Figure 6.
We also fix the membrane by the vestibular side, achieving adequate stability of the same on the bone defect.
-
Figure 7.
Summary of membrane manipulation and bone grafting, until obtaining compact and stable regeneration.
-
Figure 8.
Tension-free primary closure through correct management of the lingual and vestibular flaps and appropriate periosteal incisions, together with the application of simple horizontal mattress sutures.
-
Figure 9.
Clinical and radiographic status of the regenerated area after 10 months of healing.
-
Figure 10.
Re-entry into bone regeneration after 10 months (after removing the membrane), achieving a compact and vascularized newly formed bone, where we will place implant 36.
-
Figure 11.
Re-entry into regeneration at 10 months. Before and after comparison, after performing GBR with NeoGen Ti-Reinforced PTFE Membrane in the defect area.
-
Figure 12.
Placement of implant 36 on the newly formed bone (occlusal view), we also performed a histomorphometric analysis of the bone tissue, obtaining 40% of vital bone.
-
Figure 13.
We performed surgery on soft tissues to gain inserted keratinized mucosa, using a free connective epithelium graft in the regenerated area, with a crestal and apical strip.
-
Figure 14.
Application of tissue adhesive on the free connective epithelial graft to improve its stabilization, because it is an area where free gingival grafts usually have a worse prognosis and/or greater contraction, largely due to the relationship of this area with the origin of the buccinator muscle.
-
Figure 15.
Free gingival graft in the maturation phase before connecting the healing abutment, and subsequently placing the rehabilitation on the implant 36.
-
Figure 16.
Comparison between the initial state of the defect in the 3rd quadrant and the gain of hard and soft tissues.
-
Figure 17.
Rehabilitation placed on implant 36, with stable tissues around it and with a satisfactory aesthetic and functional result.
-
Figure 18.
Comparison between the initial state of the defect and the gain in hard and soft tissues with the rehabilitation in place.
-
Figure 19.
Periapical radiograph where we observe the gain in bone tissue in relation to the initial state.
-
Figure 20.
Panoramic X-ray one year after placing the rehabilitation on implant 36, where the gain in bone tissue in relation to the initial state and its stability can be observed.
"NeoGen membranes are specially designed to regenerate large three-dimensional bone volumes in a predictable way, thanks to their double PTFE texture and their great capacity to maintain space, due to the great rigidity of their titanium mesh, providing the appropriate conditions for effective bone neoformation.“
Downloads
Downloads
-
Regenerative Materialien




















